You can reverse symptoms of pelvic dysfunction naturally!
10 minutes/day is all you need to get started from home
Hypopressives Training Course
With the Hypopressives breath-hold, get back to doing things you love with no limitations.
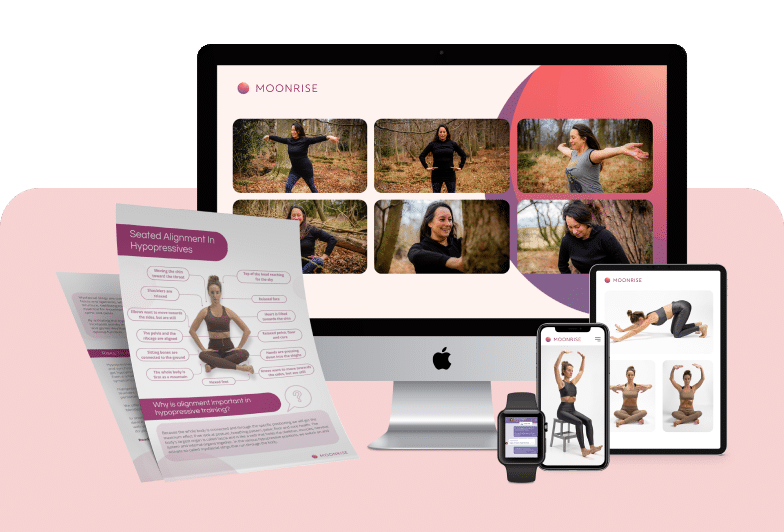
- 10 mins/day videos to follow-along
- 1:1 support from a hypopressives instructor to ensure you are doing the technique right
- Live weekly classes that are affordable and catered to different time zones
The Complete Pelvic Dysfunction Program
12-weeks completely tailor-made program with multiple natural therapies
- 10-20 mins/day videos to follow-along
- +15 practitioners from around the world
- Covers physical exercises, lifestyle & mind over medicine techniques
- 1:1 coaching throughout the period.
She is there every step of the way, including supporting you emotionally! - Live weekly classes that are affordable and catered to different time zones
Perfect for women looking for a comprehensive program to start healing fully! Requires between 15-30 minutes/day.
Why our programs work?
1:1 Support personalized to your needs
LIVE weekly classes and group calls
Continuous updates of content and new therapies
On-demand video library, any time, any device


Here are answers to questions you might have
Yes Hypopressives can help with these symptoms and other connected conditions affecting our core, back & pelvic health.
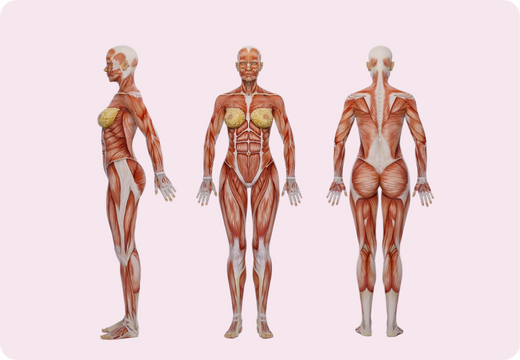
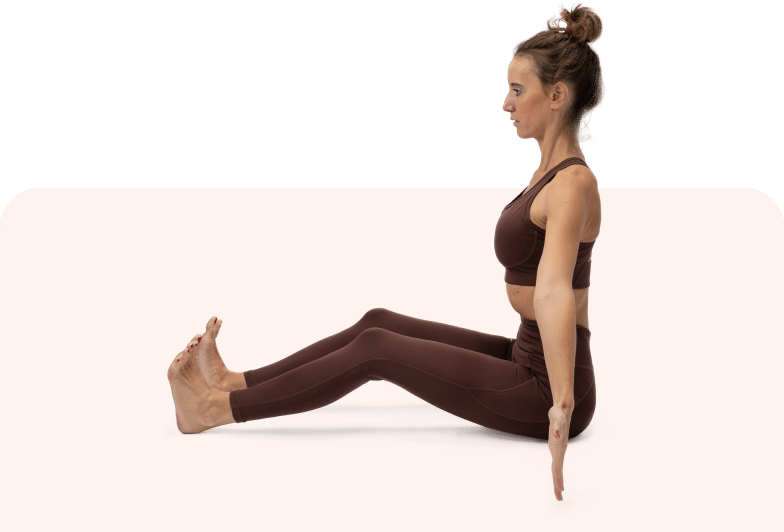
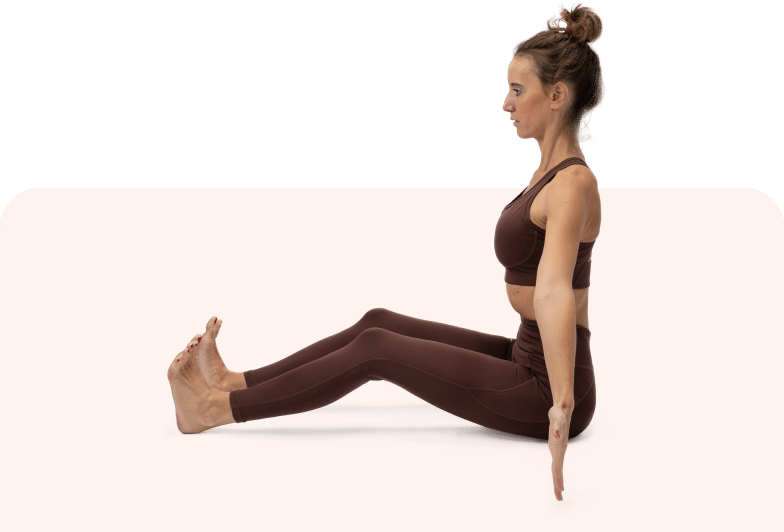
Hypopressive exercises combines various positions of the arm and feet along with the apnea or breath hold to activate your myofascial slings.
Myofascial slings are complex connections of muscle, fascia, and ligament, which help support the inner, stabilising muscles (deep supportive core) of the trunk and significantly contribute to movement and stability of the lumbar spine and pelvis. Every single Hypopressive helps you rejuvernate and reconnect your pelvic floor and core naturally.
Hypopressives require no equipment and are suitable for women of all ages and conditions. With tons of modifications available, you are never left behind with Hypopressives.
Read about all the symptoms Hypopressives helps with here
As you can imagine, the answer is very individual.
Some women notice a change after 3-6 months. Some after 3-6 weeks. We know you are eager to reach better health, yet we see the best results in women not expecting to see results, but who keep doing the work no matter what.
If you have a limited budget & time, we recommend beginning with our Hypopressives Course. You only need 10 minutes/day and for a 1-time payment of 119 USD, you get lifetime access to all content, live classes & 1-1 support to ensure you are doing the technique right.
If you need more 1-1 support, access multiple therapies and can spend more resources, we recommend our full signature Pelvic Floor Dysfunction program with Filippa. In this 12-week program, you get the following:
- You get Filippa working 1-1 with you.
- You have access to multiple therapies (Hypopressives are included)
- You would start with 10 minutes/day and slowly get up to 30-45 minutes/day of self-healthcare work.
- The 12-weeks gives you the opportunity to dive head first to reclaiming your health
- You can also pause the program for up to 8 weeks since life happens and this should not feel stressful.
We tend to see better outcomes as you add more therapies to your toolbox to reverse symptoms.
Buy Pelvic Dysfunction Program with Filippa
Still unsure? Take this quiz to get your recommendation:
Yes! Our healing programs are built on 3 foundational pillars of lifestyle changes, body-based practices & mind over medicine that work for all age groups. Our latest cohort’s average age was 63.
In short, women of all ages see results when following our guidance and the methods in our programs.
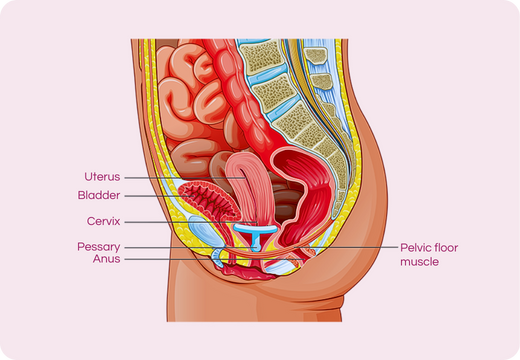
A hypertonic pelvic floor is an overactive, highly tensed pelvic floor. Doing more Kegels here would be detrimental since it creates more tension.
While relaxation is the way to go, you need to aim for a reflexive pelvic floor i.e. a pelvic floor that supports you in your everyday movements and in your everyday life.
Our program helps you get there by decompressing pelvic tension and helping you relax the pelvic area and the rest of your body by activating the parasympathetic nervous system.
Yes, Hypopressives can work even if you have been operated for pelvic dysfunction/prolapse. If you have recently been operated, we recommend getting a certificate to get started working out again from your doctor. Until then, we recommend only doing the lateral breath & alignment, and not the apnea.
Yes, Hypopressives can indeed help with overactive bladder & incontinence. We see women experiencing these results with consistent practice 10 minutes/day for 3-6 months.
If you are joining us since you are not seeing results from Kegels, we would recommend you to avoid Kegels for the time you try our program/Hypopressives. Hypopressives & our other programs activate the slower muscle fibers, fascia and nerve threads that we don’t activate when we do a Kegel. We also think it is a cleaner approach to understand if Hypopressives/our program is working for you.
Yes. Constant Hypopressives can help you get a better recovery after your pregnancy. However you are recommended not to do the apnea breath if you are pregnant. You are welcome to do lateral breath & alignment which really constitute the 80% of the technique and benefits.
Yes with the right set of personalized exercises, Diastasis can indeed be reversed years later.
The key to getting this right is to ensure the following:
- You have measured your separation right (we teach this in our program)
- You listen to your body and follow the exercises safely
- You communicate with us if something doesn’t feel right
- You are consistent in your practice (90-180 days, 10 mins/day)
- You give your body the right support mentally and emotionally.
You use a set of body-based practices created specifically for women with Diastasis Recti (DR) that are both safe and proven to work. They work because they address the root cause of this condition – which is the overstraining or damaging of the linea alba (connective tissue) located in your abdomen. Plus, when you add in some mind-based & lifestyle practices to these physical DR exercises, you create an environment where you can accelerate your healing.
Tips and tricks to reach peak feminine health
Join over 60,000 women who read our articles every week.
Get your health back from your home
Start getting better today
Hypopressives Training Course
With the Hypopressives breath-hold, get back to doing things you love with no limitations.
- 10 mins/day videos to follow-along
- 1:1 support from a hypopressives instructor to ensure you are doing the technique right
- Live weekly classes that are affordable and catered to different time zones
The Complete Pelvic Dysfunction Program
12-weeks completely tailor-made program with multiple natural therapies
- 10-20 mins/day videos to follow-along
- +15 practitioners from around the world
- Covers physical exercises, lifestyle & mind over medicine techniques
- 1:1 coaching throughout the period.
She is there every step of the way, including supporting you emotionally! - Weekly Live classes
Perfect for women looking for a comprehensive program to start healing fully! Requires between 15-30 minutes/day.